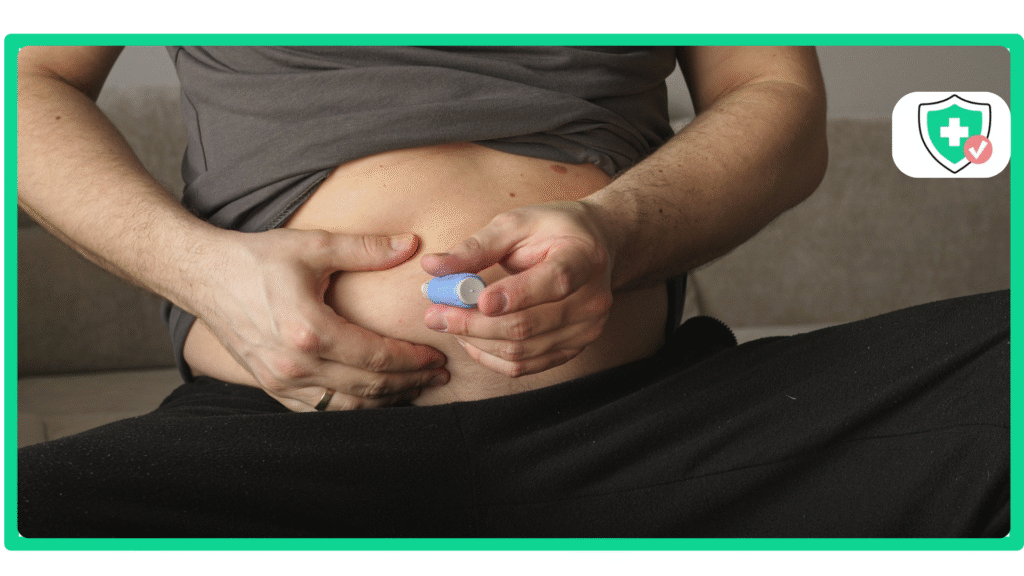
If you are part of a military family, you know that understanding your healthcare benefits can sometimes feel like a real challenge. The rules can be confusing, and it can be hard to get straight answers. A medication that many people are talking about right now is Semaglutide. It’s used to help with both Type 2 diabetes and weight loss. This leads to a very important question for military families: does Tricare cover semaglutide?
The answer is not a simple yes or no. It depends on why you need the medicine and which brand name it is. This article will break it all down in a simple way.
The Most Important Factor: Your Diagnosis
When it comes to Tricare, the reason your doctor prescribes a medicine is the most important thing. This is especially true for Semaglutide.
Semaglutide for Type 2 Diabetes (Ozempic®, Rybelsus®)
If you have been diagnosed with Type 2 diabetes, Tricare will usually help cover your medication. This is because treating diabetes is considered “medically necessary.”
For this reason, brand names like Ozempic and Rybelsus are often on the Tricare formulary semaglutide list. A formulary is just the official list of drugs that Tricare agrees to help pay for.
However, you will almost always need something called a prior authorization. A Tricare prior authorization semaglutide form is paperwork that your doctor has to fill out. It explains to Tricare why you need this specific medication for your diabetes.
Semaglutide for Weight Loss (Wegovy®)
This is where things get tricky, and it’s the answer most people are looking for. For a long time, Tricare has had a rule that it does not cover medicines that are only for weight loss.
Even though Wegovy is the brand name of Semaglutide that is FDA-approved for weight loss, Wegovy Tricare coverage is usually not available. This is because it falls under that weight loss rule. So, if you are prescribed Semaglutide only to lose weight, Tricare will likely not cover it.
Why Is There a Difference? Medical Necessity vs. Lifestyle
You might be wondering why Tricare would pay for the same medicine for one person but not for another. It all comes down to how insurance companies think.
Tricare and many other insurance plans see treating a disease, like diabetes, as medically necessary. This means it’s something they have to help you with to keep you healthy.
On the other hand, they have often called weight loss drugs “lifestyle” medicines. They see it as something extra, not something that is fixing a disease. Even though many doctors now see obesity as a disease, the insurance rules have been very slow to change.
How to Check Your Specific Tricare Plan
The best way to know for sure is to check for yourself. Here are three simple steps you can take to get a clear answer.
Step 1: Use the Tricare Formulary Search Tool. This is the official website where you can type in the name of a drug and see if it’s on the list. It is the best place to start.
Step 2: Talk to Your Military Doctor. Your doctor knows your health best. They can tell you if you have a medical reason for the prescription and can help you with the prior authorization paperwork if you need it.
Step 3: Call Tricare Directly. If you are still confused, you can call the phone number for your Tricare region. This allows you to talk to a real person who can look up your plan and give you the right information.
Alternatives If Tricare Denies Semaglutide Coverage
It can be very frustrating to be told that your insurance won’t cover a medication you need. But it doesn’t have to be the end of the road. There are other options. This is where telehealth companies offer a modern, simple solution.
Consider Sarah, a military spouse who wants to focus on her health. She finds navigating the Tricare paperwork confusing and is told her plan won’t cover Wegovy for weight loss anyway. Instead of giving up, she discovers that a direct and accessible path to treatment allows her to get a medical consultation and medication without all the insurance hurdles.
This is a great place to talk about alternatives if Tricare denies semaglutide. These programs are built to be easy.
We believe getting the care you need should be simple. Our transparent program at Semaglutide Medics is designed to be a straightforward and affordable solution, with a flat rate of just $299 per month. This all-inclusive cost covers your medical consultations, the prescription medication, and free delivery directly to your home. Start your free, no-obligation consultation to see if you are a candidate, all from the comfort of your home.
Conclusion: So, Does Tricare Cover Semaglutide?
Let’s wrap up with a clear answer. The question “does Tricare cover semaglutide” really depends on your diagnosis. In most cases, it is covered for Type 2 diabetes with special approval, but it is usually not covered for weight loss alone.
The most important thing you can do is check the official Tricare formulary and talk to your doctor. They will have the best information for your situation.
And remember, even if your insurance plan says no, it doesn’t mean you are out of options. There are other clear and affordable ways to get the treatment you need to reach your health goals. If you have questions about our program, contact our dedicated care team today.
Sources: